Mindful Eating, or Listening To Your Body’s Hunger Signals
By Juliana Ronn, First Mile Care, Director of Operations
“Mindfulness” has become a popular concept in the last few years as a healthy strategy for dealing with our stress-filled lives. When practicing mindfulness, you focus on the present moment. You concentrate your awareness on your current thoughts, feelings, bodily sensations, and surrounding environment. Mindfulness is often linked to calming techniques like meditation.
Did you know that you can apply mindfulness techniques to eating? The close connection between your stomach and your brain can be influenced through the practice of mindfulness. Mindful eating is learning to listen to your body’s natural hunger cues so that you eat when you experience true, physical hunger and not just the hunger that originates in your head that is affected by your emotional state.
Coach Kathy Gregory recently offered a short training in mindful eating as part of the First Mile Care Diabetes Prevention Program (DPP) webinar series on “Diabetes Prevention in Action.” Kathy is a holistic health and wellness coach certified through the Institute for Integrative Nutrition.
Can You Hear Your Body Speak?
Identifying the key triggers for your eating can help you understand the true message your body is trying to tell you. In this webinar, Kathy reviews the questions to ask yourself to gauge if you’re eating emotionally, how to assess your cravings on the Hunger Scale, the value of logging your daily intake in a food journal, and how to practice eating mindfully.
As Coach Karalyn Cass noted in our earlier Food Journaling webinar, your body naturally tells you when you’re hungry, and warns you when it’s time to stop eating. Unfortunately, we often ignore the signals. Becoming more mindful of the sight, smell, touch and taste of your food will slow down your eating, give your stomach time to connect with your brain, and help you to interpret your body’s natural signals.
Mindful eating requires practice to be effective. Listen to the audio recording so you can follow along as Coach Kathy explains how you can develop control over emotional eating. She’ll take you through a mindful eating exercise, so be sure to have a healthy snack on hand!
To learn more about how you can benefit from the First Mile Care Diabetes Prevention Program, take our prediabetes risk test and get started today!
Easy Meditation Techniques for the New Age of Anxiety
By Juliana Ronn, First Mile Care, Director of Operations
Are you feeling disconnected from your normal activities? Do you have restless nights? Perhaps you obsessively “doomscroll” through Twitter before bedtime?
You’re far from being alone. Many of our usual habits have been uprooted by COVID-19. We are spending more time at home, and going out can often lead to worry about putting ourselves at risk. Feeling heightened anxiety and stress as a result of the pandemic has become many people’s normal state.
Chronic anxiety and stress can cause an overabundance of glucose in the bloodstream, as you probably know if you’re already following the First Mile Care Diabetes Prevention Program (DPP). This in turn can increase your risk of developing type 2 diabetes, as explained in an earlier article on our blog.
You can bring down your anxiety levels through healthier coping strategies such as exercise and calming techniques like meditation and mindfulness.
First Mile Care DPP Coach Lizzie Nichols recently offered a short training in simple meditation and relaxation exercises as part of our “Diabetes Prevention in Action” webinar series. Lizzie is a licensed family therapist with a master’s degree in counseling psychology. She is also a long-time practitioner of yoga and meditation.
Download the audio file and listen as Coach Lizzie demonstrates her meditation techniques while sitting in a chair or lying down. She guides you through short breathing and body exercises that will easily fit into a busy schedule.
Namaste!
To learn more about how you can benefit from the First Mile Care Diabetes Prevention Program, take our prediabetes risk test and get started today!
MacGyver It: How to Do Resistance Training at Home with Household Objects
By Juliana Ronn, First Mile Care, Director of Operations
If you’re following the First Mile Care Diabetes Prevention Program (DPP), you already know that a core principle for reducing your risk of developing type 2 diabetes is to perform 150 minutes of exercise per week. Yet it’s been a challenge for many people to do so during the COVID-19 shutdown of gyms, yoga and dance studios, community centers, and other shared exercise environments.
First Mile Care DPP Coach Lizzie Nichols provided useful advice for staying active while sheltering in place in an earlier article. As we slowly emerge from isolation into the “new normal,” some folks are understandably reluctant to jump back into group exercise environments, especially if they’re at high risk from the coronavirus due to age or chronic conditions. While walking and running remain great activities, they don’t replace weight-lifting and other resistance training, and not all of us have the money or space to have gym-level equipment at home.
Our First Mile Care DPP Coach Sandra Huskey recently made “at-home resistance training” a topic in our ongoing series of “Diabetes Prevention in Action” webinars. As Sandra notes, whether or not there’s a gym in your future, it’s easy to do resistance and balance training at home. Sandra is a certified group fitness instructor, so read on for her expert advice!
Your home is your gym
Resistance training is anything that uses force or resistance against your movement. At home, you can do this by using your own body weight or by using free weights like dumbbells. You can increase your resistance as you become stronger and more flexible.
But what if you don’t have dumbbells, and can’t buy any now while many stores are shut or have items on backorder? Just “MacGyver it” with your own furniture and pantry items!
-
Makeshift weights. Go into your kitchen cupboards. Soup cans and water bottles each weigh a little over a pound apiece, so with one in each hand, voilà, you have a set of weights! Soup cans tend to be a little thick to grasp, and water bottles, while slimmer, can be a little bendy. If your hands are big enough and strong enough, hold two water bottles in each hand for two pounds on each side. As you get stronger, you could work up to using a gallon jug of water or milk, which equals about eight and a half pounds.
-
Bicep curls and arm raises. Sit in a firm kitchen chair to do bicep curls and arm raises while holding your makeshift dumbbells. Do about five to ten repetitions, if possible, and then take a 30-second break. That’s called a set. Ideally, you do two to three sets of five to ten repetitions. (That advice applies to all the following exercises.)
-
Modified wall pushups. Pushups work out your chest, back, and core, so are a great all-around exercise. You probably think you can’t do a pushup — but have you tried a modified pushup? Use a flat wall, door, countertop, or another solid surface in your home to push against. Be careful to avoid any furniture item or surface that can move, such as a chair, coffee table, or ottoman, as they’re not stable.
-
Steps pushups. If you’re in a single-level home, you probably won’t have a staircase but you may have a front porch with steps. It’s pretty easy to find stairs somewhere while you’re out on a walk. You can do pushups and dips on steps to work out your shoulders, biceps, and triceps. Start on the fourth or fifth step and push against each step as you move down.
-
Stork and ballerina balancing. As you get older, it’s normal that your balance and flexibility start to waver and you may occasionally feel a little unsteady when out for a walk. With one hand on a firm kitchen chair for safety, do your best stork pose and practice lifting one leg and balancing on it. The key is to be able to take your hands away from the chair and hold your balance on one leg, starting at a few seconds and building up to a full minute. You can also use the chair for support when doing toe raises, where you lift yourself up onto your toes and try channeling your inner ballerina.
-
Hall tightrope. Another great balancing exercise is to walk down your hall or living room in a straight line as if you were on a circus tightrope or Olympics balancing beam. Start with your heels and roll onto your toes, high-stepping one foot in front of the other.
Mix it up
When you do weight training, you want to give your muscles time to rest. If you do full-body resistance training one day, try a different form of exercise the next day, like walking. Or you can alternate upper- and lower-body training on successive days.
These are all simple resistance exercises that you can do in the comfort of your own home, with tools and equipment already available to you. Balancing exercises are especially easy to practice while you’re multitasking at home, such as cooking in your kitchen. As you gain strength, continue to escalate the weight, force, and resistance you use and you’ll see progress in your strength, balance, and flexibility.
Watch First Mile Care DPP coach Sandra Huskey demonstrate these simple at-home resistance training techniques in our recent webinar.
To learn more about how you can benefit from the First Mile Care Diabetes Prevention Program, take our prediabetes risk test and get started today!
Who Says Healthy Side Dishes Can’t be Delicious?
By Juliana Ronn, First Mile Care, Director of Operations
First Mile Care has been excited to offer an ongoing series of “Diabetes Prevention In Action” webinars to help our Diabetes Prevention Program (DPP) participants stay engaged, connected, and focused on their goals during the turbulent times of the COVID-19 pandemic. These online events have already proven to be a successful way for our coaches to utilize their expertise, digging deeper into topics that can only be briefly covered during normal DPP sessions.
A recent entry in this webinar series saw Coach Irazema Garcia share her technique for making perfectly roasted cauliflower with lemon tahini sauce. Healthy eating is a topic close to Irazema’s heart, as she specialized in holistic nutrition as part of her master’s degree in health education.
Vegetables make up a critical part of a healthy, pre-diabetes diet and can help keep you from developing type 2 diabetes. They are low in calories and high in vitamins, minerals and fiber. Irazema notes that cauliflower in particular is a rich source of fiber, potassium, vitamin C, and folate. Enjoy it mashed, roasted, riced or even as pizza crust. It is a real powerhouse when it comes to versatility and nutrition.
The delicious tahini sauce adds healthy fats to your veggies, which can also boost their nutrient value. Plus, adding a little fat helps you feel fuller for longer.
Irazema’s recipe works as an amazing side dish, snack, appetizer or centerpiece of the meal. Enjoy!
Roasted Cauliflower with Lemon Tahini Sauce
-
2 cups cauliflower florets
-
2 tbsp tahini
-
Juice of half a lemon
-
1-2 tbsps. cilantro, chopped
-
1⁄4 tsp smoked paprika
-
1-2 tbsps. olive oil
-
water
-
pink salt
-
black pepper
Directions
-
Preheat oven to 425°. Toss florets with olive oil, salt, and pepper making sure to coat well.
-
Place cauliflower in a single layer on a baking sheet.
-
Roast for 15 minutes or until slightly charred.
-
Meanwhile mix tahini, lemon juice, salt, and paprika.
-
Add water as needed (about 2-3 teaspoons) to smooth out the sauce. The end result should be lump-free and pourable, but not watery (think ranch dressing).
-
To serve: plate cauliflower and drizzle with lemon tahini sauce, then sprinkle liberally with cilantro and black pepper.
Download the recipe here.

To learn more about how you can benefit from the First Mile Care Diabetes Prevention Program, take our prediabetes risk test and get started today!
A Journey of Self-Discovery Through Mood-Food Journaling
By Karalyn Cass, First Mile Care, DPP Coach
The COVID-19 pandemic has disrupted our lives in so many ways. Your eating habits have undoubtedly changed from what they were in pre-coronavirus days. You may be eating more home-cooked food, but also snacking throughout the day to combat stress, boredom, or loneliness.
Keeping a food journal is an effective tool to help you learn about your “new normal.” Not only does food journaling track the calories you consume, it reveals trends and patterns in your eating habits that affect your risk of developing type 2 diabetes. It highlights the foods and beverages you most often consume, how much is healthy versus unhealthy, and the link between what you eat and your emotional state. That information will help you to evaluate your behaviors and set reachable goals for changing them. In fact, a research study involving 1,700 participants determined that the people who kept daily food logs lost twice as much weight as the people who didn’t track their food intake at all.
There is also an accountability factor to food journaling. It may subconsciously discourage you from careless eating because you have to write down every snack in your food log. If you’re in the First Mile Care Diabetes Prevention Program (DPP), you’ll also discuss your journal findings with your DPP coach and neighborhood class participants, who can help you come up with strategies to cope with your eating triggers. Food journaling is a great self-discovery tool that helps you to investigate your relationship with food and its connection to your mood.
How to keep a food journal
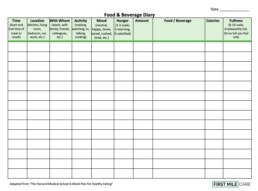
Some people believe food journaling can be tedious. However, the self-discovery is so eye-opening that many people love it. For basic tracking of your food intake, you can go the traditional route of using paper and pencil to keep a food log.
You can also use the voice recording feature on your phone. A convenient digital way to track your food intake is through apps on your smartphones and computers. Lose It!, My Plate, and MyFitnessPal, among others, allow you to note your activities and track calories by breaking down ingredients into carbohydrates, proteins and fats. There are even photo-recognition apps now such as Foodvisor and Bitesnap that can calculate the calories of the food in a photo of your meal.
Whether it’s a paper spreadsheet, an app, or a combination of the two, it’s important that you keep a food journal for at least a week to become familiar with your true eating habits. Making journal entries as soon as possible after eating will result in more accurate details.
8 questions to ask yourself when food journaling
Food journaling goes beyond mere meal tracking. It’s not simply about counting calories. Journaling is connecting the dots between what you eat and how you feel throughout the day — both your food and your mood. You’ll track details about your meals and snacking such as the time of day, where you are, who you’re eating with, how hungry you are, and how quickly you become full.
Record answers to these eight questions in your food journal:
1. What are you eating? Not only do you record the food or the beverage that you’re consuming, but also any of the sauces, dressings, condiments, and toppings. Your caramel macchiato has vanilla syrup and steamed milk as well as coffee. The preparation details of your meat and vegetables are important — was it baked, boiled, fried, grilled or steamed?
2. How much are you eating? Try your best to estimate how much you are eating using standard household measurements (cups, ounces, teaspoons). Try weighing your food for a trial period to get a better idea of your servings. Some smartphone apps have databases that will do calorie calculations for you.
3. When are you eating? The time of day that you eat can be very insightful in identifying potentially problematic behaviors such as late-night snacking or that midday slump. Knowing exactly when you are most likely to feel hungry is important for adjusting your eating schedule and frequency, so you can avoid overeating as a result of waiting too long to eat.
4. Where are you eating? Take note of the location of where you eat — whether it’s your dining table, the living room, your office, your car, a restaurant, a friend’s house, or even walking down the street.
5. What are you doing while you’re eating? Multitasking and eating can be a recipe for disaster. It can make it easy to ignore your body’s signals telling you that you’re full. Try eating a meal without TV and phone screens as a distraction, so that you concentrate on the taste and texture of every bite of your meal.
6. Who are you eating with? Americans eat and drink alone more than half the time, according to research. Studies have also found that solo diners are also more likely to eat at irregular times and consume unhealthier foods with fewer fruits and vegetables. Eating with others tends to put you on a schedule and to eat more slowly while conversing. People also take cues from dining companions as to what to eat, and how much.
7. How are you feeling while you’re eating? Are you eating when you’re tired, bored, frustrated, anxious, sad or happy? You may find that you’re eating when your emotions tell you to eat rather than when your body tells you, or that your mood is affected by hunger. Think of being “hangry,” when you’re grumpy-angry because you’re hungry.
When you’re feeling stressed or depressed, it’s normal to crave unhealthy, high-calorie treats. During the COVID-19 shutdown, grocers are seeing a surge in demand for sugary cereals, frozen pizza, mac and cheese, salty chips, and other processed “comfort foods.” Unfortunately, stress-eating can become a vicious cycle as fat and sugar only increase the likelihood of depression and anxiety, which then causes you to want more junk food to stave off your dark mood. But keep in mind that just as unhealthy food can contribute to depression, healthy food can boost your mood.
8. How hungry and how full are you?
It’s important to be mindful of your hunger cues so that you pay attention to true, physical hunger and not the hunger that’s in your head caused by emotions. Your body naturally tells you when you’re hungry, and warns you when it’s time to stop eating. In your food journal, rate your hunger level every time you eat on a “hunger scale” between 1 and 10, where 1 is starving and 10 is so full that you feel sick. To eat naturally, the way a baby eats, you want to eat when your hunger is at a 3 or 4. It takes about 20 minutes for your brain to recognize that you’ve eaten enough, so to avoid overeating, slowing down eating and even stopping to assess your hunger level mid-meal will give your body time to catch up.
Fitting food journaling into your life
After completing a week of food journaling, look for trends across the data in your food journal. Are you making healthy choices? Are you reaching for a snack when you’re bored? Do you overeat when having a meal in the kitchen near the fridge? How often are you eating while on the run? Is watching TV a trigger for evening snacking? Should you eat more frequently to avoid overeating when you’re extremely hungry?
The longer you keep a food journal, the more you’ll discover about your eating habits. You will then be able to create a successful strategy for recognizing your hunger cues and consistently make healthy choices. Give mood-food journaling a try!
To learn more about how you can benefit from the First Mile Care Diabetes Prevention Program, take our prediabetes risk test and get started today!
Traveling Along the Road to Better Health through DPP
By Tappan Dearrigunaga, First Mile Care DPP Participant
I joined the First Mile Care Diabetes Prevention Program (DPP) at the recommendation of my general care physician, Doctor Savant, in whom I have great trust. I figured the coach would fix me, the way a mechanic fixes a car. I thought I would learn about blood sugar and exercise and be given set goals. But that’s not how First Mile Care DPP works. It’s not an event; it’s a journey.
When I started the program, I was pretty confident that my current diet already left little room for improvement. I had been diagnosed with prediabetes nearly a decade before and since my sugar levels hadn’t tipped into full-blown diabetes, I assumed I was doing — if not great, at least good enough. But my prediabetic state, combined with other factors, had a destructive impact on my health.
In the beginning, I was dubious of the results I would see from the program. It seemed too simple as the steps my coach recommended were very basic things. You start small. You develop a personalized action plan and track eating, exercise, and other details in a notebook.
My phenomenal DPP coach has helped me to become aware of the areas of my life that could be improved. Her thoughtful guidance led me to personal insights into specific, sustainable changes I could make. We were able to create a set of realistic goals for diet and exercise that I could commit to because they were tailored to my needs.

New habits for a healthier lifestyle
As the weeks progressed, the incremental tweaks to my behaviors resulted in real, noticeable changes. My coach was passionate about prompting me into learning how to modify my habits to result in a healthier lifestyle. I tracked not only how often I was exercising but the type of exercise, the intensity, and the duration. I increased lean muscle mass, reduced fat, and lost a significant amount of weight.
I also became hyper-aware of what I was eating, and how much, and what triggered my craving for certain foods and drinks. I was surprised at how much processed sugar and corn syrup are in some of the foods that I thought were fairly healthy – such as the majority of breads. Learning to examine nutrition labels in order to reduce my consumption of processed foods with high salt, sugar and fat content was a challenge at first. But it eventually became automatic, and once I found healthier substitutes, I quickly saw positive results. I ate less because I was no longer eating “hollow foods” with poor nutritional value that left me always wanting more. I even started using smaller plates because I felt well-nourished by smaller portions of nutrient-dense foods.
The power of the tribe
One of the most effective components of the First Mile Care DPP program is what I refer to as “the power of the tribe.” It’s a small group in the same community — mine was a half-dozen people — that meets in a convenient neighborhood location to share goals and encourage each other to be successful. The group setting was paramount to my own personal success with DPP. The power of sharing my struggles and successes with a group of people with whom I’m on a first-name basis, and who have similar goals for changing their lives, was exponential.
In the first six months of the program, the weekly meetings acted as an anchor for me, as I knew I had to be accountable for the progress (or lack of it) that I’d documented in my notebook. But I also knew my fellow travelers wouldn’t judge me if I’d slipped up and would empathize as they shared their own struggles. It’s encouraging to see other participants making progress, which was especially noticeable in the second half of the program when the group meetings switched to a monthly schedule. And because we lived in the same area, we could even meet up outside regular group settings for support, if needed.
Whenever those moments occur where I’m tempted to go back to my old habits, I think of the other group participants and my First Mile Care coaches, all of whom are still available to support me. They have become my friends — relationships I expect to keep for life.
I now eat better, sleep better, and feel better overall. As a result, I am also happier, and this positive mood rubs off on those around me.
Preventing diabetes is not a quick fix. There is no real finish line. I realize now that my prediabetes journey doesn’t end when the First Mile Care program is over. Instead, my DPP coach has given me the tools I need to self-manage my behaviors and maintain my journey to a healthier lifestyle — now and for the rest of my life.
To learn more about how you can benefit from the First Mile Care Diabetes Prevention Program, take our prediabetes risk test and get started today!
Staying Active While Sheltering at Home
By Lizzie Nichols, First Mile Care, DPP Coach
Staying active for 150 minutes a week is a core principle of First Mile Care and the Diabetes Prevention Program (DPP). When we find ways to increase activity, we reduce our risk for developing diabetes. We face enormous cultural changes due to the Coronavirus (COVID-19), with many of us directed to “shelter in place” as well as practice social distancing. Therefore, many of our usual resources for staying active (gyms, community centers, yoga studios, and more) are closed to in-person business. On a positive note, there are still plenty of ways we can get adequate physical exercise at home and a lot of our local resources are offering virtual classes.
Benefits of Physical Activity
As we face the challenges of isolation and working from home, it is important to remember the benefits of physical activity to stay motivated and meet our goals.
-
Lower stress and lift mood
-
Better sleep
-
Control weight
-
Improve cholesterol
-
Lower blood pressure
Action Plans
In our weekly DPP meetings, we focus on an “action plan” to make the small changes around nutrition and exercise that will facilitate the lifestyle changes to prevent pre-diabetes. We encourage you to lean into your action plan as you navigate new ways of increasing exercise while sheltering at home. Identify small, specific, realistic and do-able goals. As always, if things aren’t going according to your plan, go easy on yourself and readjust.
Schedule It
There is a strong inclination to keep to a schedule as we develop a new structure for our days at home that addresses both work and family obligations. We can use this for exercise as well. You can identify longer activities, like a 30-minute walk, and schedule it three times a week. Or you can choose shorter intermittent activities, like 10-minute building strength exercises, and do them three times a day. Pick the activity structure that works best for you and your family.
Home Activities
Hopefully, there have already been some changes that you have been able to implement at home. We always encourage using what you already have on hand.
-
Your body is always available for squats, wall push-ups, sit-ups, lunges, crunches, planks, and more
-
Yoga and Pilates aerobic workouts online and on fitness apps
-
If you already have cardio equipment at home, jump on!
-
Virtual games and Wii Sport
-
Family dance parties or virtual ones while videoconferencing with friends
-
Climb the stairs into or inside your home
-
Do household chores to music and put a little more pep in your step
Outdoor Activities
It is still possible to exercise outdoors with six feet of safety between you and a family member or friend. If you feel comfortable and the weather is fine, taking yourself outdoors is a pleasant way to lift your spirits while maintaining human connections.
-
Gardening
-
Walking (or walking your pet)
-
Hiking
-
Jogging
-
Biking
Online and Local Resources
Individual instructors and businesses are finding creative ways to bring their classes online. Be sure to check with your local resources to see what they are offering, either fee-based or as freebies. If you can’t find anything in your community, there are many offerings through national organizations such as the YMCA. Even celebrities are offering free workouts and dance lessons through social media.
Stress and Diabetes
By Irazema Garcia, First Mile Care DPP Coach
Stress and stressful events are part of modern life. We acknowledge it, and sometimes even equate it with success: Ever bragged about working 60+ hours a week just to get that project completed? Stress has its purpose — like when you have to slam on the brakes to avoid a collision or whip your hand from a hot stove to avoid a burn. But what happens when there is too much stress in your life?
Stress-Diabetes Connection
Stress triggers the sympathetic nervous system, activating the fight-or-flight response. This response quickly raises the body’s source of energy — glucose or blood sugar— to help either fight the danger or flee from the danger. This comes in handy when we are faced with a physical threat that might result in a life or death situation. But when the body does this in reaction to chronic stress (stress that happens frequently), an over-abundance of glucose begins flooding the bloodstream. Over time, this can keep glucose levels consistently elevated in the blood stream, leading to prediabetes and perhaps even diabetes. Lowering chronic episodes of stress can, in turn, help regulate blood sugar.
Physical threats to survival were greater for early humans. Today, very few daily stressors require us to fight or flee. Running away from a conference call or a presentation is rarely the wisest option. Neither is sprinting to higher ground when the kids are screaming. And there is no way to win a battle with heavy traffic on the way to work.
Our bodies’ cannot discern between being chased by a saber-toothed tiger and dealing with the morning commute. If we need to outrun a predator or climb from rising flood waters, glucose supplies the necessary energy to do so in order to keep us safe. The surge in glucose gives the body an optimal chance of surviving the threat by giving cells more energy to run or fight (or both). However, in the case of chronic stress — the kind that elicits a stress response for more than a few moments —the body steadily sends out glucose which ultimately takes a toll on the body.
More Ways Stress Affects Blood Sugar Regulation
Stress can also play a role in lifestyle choices. It leads many people to find comfort in certain foods — generally high-carb, high-caloric fare. “Comfort food” is called that for a reason; it’s commonly associated with soothing emotions. However, those foods also generally raise blood sugar, opening another route for prediabetes and diabetes to develop. By any terminology, too much “comfort” or “stress” eating hinders blood sugar regulation.
Chronic stress can also be associated with fatigue and depression, which can cause people to become less active and lead more sedentary lives. This lack of movement can prove to have a negative effect to prediabetes and diabetes risk because an inactive lifestyle is also detrimental to blood sugar regulation (the more we move, the more glucose is expended).
Ways to Destress
Everyone has different methods to calm stress. Some people find it tranquil to be quiet and alone, while others find the best way to decompress is to be around others. There is no right or wrong way to relax. Below are few ways to destress that may prove beneficial:
-
Shift Viewpoint: Although little can be done in modern-day society to limit traffic or work deadlines, shifting your viewpoint can help lower stress. You may not be able to change the world, but you do have the ability to change your reaction to the situation at hand. Start by visualizing how you can reframe stress-inducing situations into something neutral or positive. Does the presentation you have to give at work need to be a nerve-wracking exercise in anxiousness? Instead, try to frame it as fun opportunity to fill your team in on what you’re working on and are passionate about.
-
Movement: Injecting physical activity into your day can help relieve stress. Do you usually feel better after a walk? Ever noticed how a run helped you figure out the solution to a problem? Movement relieves muscle tension and facilitates deep breathing — both great factors in decreasing stress. Movement also releases endorphins – the neurotransmitters that make you happy, which can aid in stress relief. Physical activity does not have to mean marathons or arduous hikes, short bursts of activity can prove beneficial as well. Any kind of movement helps.
-
Ignite the Relaxation Response: Whether it is through deep breathing, yoga, or visualization (or anything else that calms the mind), the relaxation response can counter stress. It helps to calm both the body and the brain down (especially that inner chatter that can compound stress). Relaxing creates an environment inhospitable to negative stress.
-
Find Your People: Having social support when times get tough reaps great benefits. The emotional support that can be received from being part of a network can reduce tension and help with long-term positive health outcomes. Whether it is finding a support group close to your home or reaching out to family and friends via social media, human support eases stress.
The stress-diabetes connection can be seen from many different angles: The positive and negative roles stress itself, can play in the body, but also the changes long-term stress induces and makes us feel.
Bottom line, one of the best actions to take in terms of lifestyle change is to find ways to destress regularly. Different things work for different people, but finding what works for you (and when) can play a crucial role in diabetes avoidance or management.
DPP: Resolutions vs. Action Planning
By Irazema Garcia, First Mile Care DPP Coach
It’s resolution time! As a First Mile Care Diabetes Prevention Program (DPP) coach, I am trained to support people through significant lifestyle change using the Center For Disease Control’s (CDC) clinically proven methods. In my DPP classes, I have noticed that come January, people customarily set out to make big changes for the upcoming year. They optimistically hope that this will be the year those good habits stick. Gym memberships are purchased. Healthy groceries are hauled home. New running shoes appear by the door.
Unfortunately, an estimated 80% of resolutions fall to the wayside by mid-February. How is it that the people who ooze with excitement for change on New Year’s Day give-up by Valentine’s? I’ve learned that people simply need to shift their mindset ever so slightly to achieve success.
Oftentimes, the reasons resolutions don’t stick long-term fall into three categories:
-
Too Unrealistic: The “over” in overachieving plays its part. People sometimes make resolutions that are very challenging to accomplish. If the goal is to run a marathon having never run before, it’s awfully difficult for most folks to hit those 26.2 miles. Disappointment makes it all that much easier to give up.
-
Lack of Intrinsic Motivation: Creating resolutions because “it’s what you do on January 1st” is not always the best option. Doing something because you feel you should rather than because you genuinely want to often yields unsuccessful results. In one exercise study, participants who exercised for extrinsic reasons (seeking an “outside” reward or outcome, such as improving appearance or reducing clothing size) were less likely to continue exercising long-term than the participants who exercised for intrinsic reasons (enjoyment of the activity, desire to achieve competence, etc.). Starting something when your heart is not in it might make it easier to stop doing it.
-
Too Vague: “I am going to lose weight” is a statement almost everyone utters in life at one point or another. Although it sounds perfectly doable, the fact that it is very vague can stand in the way of actually achieving the goal. How much weight? What is the marker of success? Is there ever an end to the weight loss? Without clear guidelines, it becomes easy to get frustrated or lose interest — not because you can’t succeed, but because you never defined what success would look like.
Action Planning
Committing to goal setting and action planning rather than resolutions can help solve these problems. Goal setting is different than making resolutions. It is effective because it focuses on actionable steps and creates a roadmap to follow for achieving a purpose, making the process clear and understandable. Using action plans, like those prescribed in DPP, leverages small and achievable goals to set up success long-term and fulfill larger goals.
So how can you ensure you are setting actionable goals rather than resolutions? Follow this three-step approach set yourself up for long-term success:
-
Get Real: Set yourself up for success by choosing realistic goals. A goal must be doable in order to be successful. If you are new to exercising at the gym, then perhaps your action plan should be 2 times a week for the first few months in order to get acclimated — not all seven days. Be honest with yourself about what you can handle. And if you have weeks where you do make it to the gym all seven days, then that is just a bonus. It is better to plan realistically and sometimes surpass the goal you set for yourself than to set unreasonably high expectations and court failure. Your self-esteem will thank you for it.
-
Identify Your Drive: Pinpoint internal motivation before setting out on your goal. Are you giving up donuts (even though you love a good chocolate cruller Sunday mornings) solely because your coworker swears he lost 10 pounds doing so? What’s really fueling your drive? Is it external or your own? Determine why you are trying to accomplish your goal (Reduce the risk of diabetes? Better quality of life? Be there for your family?). Find that intrinsic motivation and embrace it. Write it down, post it on the mirror — whatever it takes to remind you of your own “why.”
-
Focus on the Process: When you set a goal, don’t obsess on the endgame. Instead, focus on the journey you will take to reach that goal. Don’t fixate on dropping 5% of your weight. Concentrate on changes you can make that will result in 5% weight loss. Immerse yourself in the process that needs to occur for weight loss to happen. It may mean reexamining portion sizes, zeroing in on nutrition information, or planning a break-time group walk with coworkers to increase your daily physical activity. Make action plans to support progress. When the focus shifts to actual steps, rather than the goal itself, the process becomes easier to navigate. These action plans will snowball week to week and reinforce your commitment, steadily advancing toward long-term success.
Perhaps most importantly, use your support network! DPP with First Mile Care is all about personal action planning tailored to the individual coupled with the fundamental truth that people have the greatest impact on other people. As every DPP coach I know will attest: The best way to propel positive action is to leverage positive support.
Goal Setting & Action Plans
By Irazema Garcia - First Mile Care, DPP Coach
Commitment is the first step toward achieving any aspiration. But sometimes, you can set out to accomplish something with great enthusiasm, only to quickly find yourself lost and confused.
It happens to all of us at one point or another. The intention is pure, but the execution can be exhausting without a clear direction. Frustration sets in. Disappointment whittles away at your resolve. Giving up starts to look promising.
You have to know what you are trying to accomplish in order to accomplish it, but getting from here to there isn’t always a straightforward journey. How can you stay on track?
Enter goal setting!
Goal setting can be beneficial because it illuminates the path and keeps the finish line in focus. Goals can pave the road to change by helping you home in on what needs to get achieved as you progress toward your objective, while filtering out what does not need to take up brain space.
Why goal setting is important
Goal setting is a fantastic way to hold yourself accountable. For example, when you’re attempting to establish a healthier lifestyle, you may set a goal to incorporate two-and-a-half hours of physical activity into your week. You then know you are trying to hit a specified amount of physical activity during a specified time period. You have a target to aim at. You are not simply running/walking/biking/etc. haphazardly each week when opportunity presents itself. You have a context. Setting a goal gives you the ability to see where you are and how you’re going to get where you want to be.
In addition, goal setting helps with momentum and self-efficacy. Hitting those milestones week after week will have positive effects on your psyche. Meeting your goals empowers you to set new goals and complete them. Suddenly, anything becomes doable. Progress becomes reasonable and plausible.
What is the purpose of an action plan?
Goal setting is particularly effective with action planning. Action planning lays the step-by-step foundation for success. If the goal is the destination, the action plan is your map.
Creating an action plan sorts out the logistics (the how/when/where) for meeting your goal. It creates a blueprint, making goals easier to reach.
In the example above, where the goal was to partake in two-and-a-half hours of physical activity, the action plan could consist of walking thirty minutes in the evening, five times a week. The action plan helps with the specifics of meeting the goal. With an action plan in place, you know you have to walk thirty minutes, five times within a seven-day window. Without an action plan, it is very easy to just say “I am going to walk” when it’s convenient and never actually hit the goal amount consistently. The action plan puts the process into motion by outlining progress that can be monitored and managed in attainable blocks.
Action planning is effective. In a randomized clinical trial, participants who incorporated action planning into changing their lifestyles were more successful in keeping-up the new behaviors and sticking with the changes they had made nine months after they started. Having that blueprint makes it easier to hit goals, and ultimately easier to keep them going. When the steps are laid out, it’s hard to get lost. And when those steps are easy to follow, it’s easier to stay the course.
How to create an action plan?
There are lots of ways to create an action plan. The best method is the one that you can keep long term. That is not to say you must stick with only one method. Test out a few different plans to see what works best for you. You can try using a phone app, pen and paper tracking, spreadsheets, a whiteboard — it is your call. There is no one size fits all when it comes to action planning or goal setting.
The important thing is to set up a goal and a plan and follow through. The plan should be specific, realistic, and attainable in order to make sure the goal is met. This does not mean you cannot (or should not) reach for the stars. It just means that larger goals may need to be broken down into a series of mini goals. Almost any goal is doable — with the right plan.