Healthy Meal Prep in the Age of Inflation, Part 2
By Jenny Fowler, First Mile Care DPP Coach
This is the second in a two-part article.
First Mile Care coaches recommend our Diabetes Prevention Program (DPP) participants eat a diet filled with fresh fruits and vegetables. We encourage folks to stay away from highly processed foods as much as possible and stick to a whole-food base when preparing meals. Shopping the perimeters of the grocery store, and focusing your food purchases in the fresh and frozen produce sections, is generally most supportive of overall good health.
Smarter shopping — fresh, frozen, bulk, and seasonal
- Shop by season. If you want to eat healthier on a budget, instead of buying what you want when you want it, embrace flexibility and buy fruits and vegetables available seasonally in your area since these tend to come at a better price. A local farmer’s market or a food co-op is a great way to educate yourself on the full variety of fresh fruits and vegetables that are in season.
- Shop by sale. I would also encourage experimenting by buying fruits and vegetables that are on sale, even if the item is not something you would usually buy! Encourage yourself to try new options to get more variety into your diet while also saving money. And if shopping at a farmer’s market, keep in mind that vendors may slash prices late in the day to avoid taking perishables back home.
- Fresh vs. frozen vs. canned. Buying canned or frozen produce is another budget-saving tip, and you can also save money by freezing fresh produce you buy in bulk. Food scientists at the University of California, Davis ran a study in 2018 to compare the nutritional value of fresh and frozen produce and were surprised to find no major differences in the overall vitamin content, especially when items are frozen quickly after harvest. Canned produce such as artichoke hearts, beets, corn, garbanzos, hearts of palm, and peppers can liven up a salad or side dish once you rinse them a couple of times to reduce salt.
- Caveat emptor. Be wary of marketing ploys. Store-brand or private label items generally have the same ingredients as their brand-name competitors but cost less. Food label buzzwords such as organic, free range, natural, and healthy are often attached to higher sticker prices. Organic foods do offer less exposure to pesticides and antibiotics, but research shows that you may derive the same nutritional benefits from frozen or fresh, or organic or non-organic blueberries, for example. The Environmental Working Group publishes annual Dirty Dozen and Clean Fifteen lists showing which foods have high pesticide residue so can be worth spending a bit more for organic, versus which are fine to buy non-organic due to low pesticide residue.
- Meatless Mondays? Consuming less meat has the benefit of not only making meals cheaper, but higher in fiber, too. Plant-based proteins such as beans, lentils, nuts, peas, quinoa, seeds, and soybean products like tofu can be purchased in bulk at a discount. If you want to keep animal protein in your diet, limit the number of days you have meat, choose cheaper cuts (enjoy a beef stew!), and use more eggs. Although eggs have shot up in price in the last year due to avian flu-created shortages, they’re generally still going to be less expensive than meat.
- Bulk up! Buying in bulk stores can save you money as long as you buy foods you can store easily, such as canned goods, pasta, rice, and spices. You’ll need to separate meat and poultry bought in bulk into smaller portions before freezing. However, it’s best to avoid buying sweet treats in bulk, to avoid the temptation to consume immediately, simply because they’re in the cupboard or fridge.
Junk temptation
When food shopping, it’s really important that you don’t allow your limited budget to steer you towards cheaper junk foods. The U.S. food supply is flooded with highly processed foods like chips, packaged breads, and soda drinks that may cost less than fresh produce, but which are loaded with fat, salt, sugar and additives. Ultra-processed foods make up nearly 60% of what the typical American adult eats, and nearly 70% of what kids eat, according to a study published in 2022 in the American Journal of Clinical Nutrition.
If the nutrition label contains a lot of scientific-sounding names that you don’t recognize — that’s a clue that the food is highly processed with flavorings, colorings, emulsifiers, and hydrogenated oils used to change appearance, texture, and taste. These foods are designed to be tasty and even addictive, while providing “empty” calories instead of quality calories that satisfy your hunger. High consumption of ultra-processed foods has been linked to obesity, cardiovascular disease, stroke, diabetes, and other chronic illnesses. Moreover, when your body is used to certain foods and you substitute them with lower quality items to save a few dollars, it can wreak havoc on the health of your digestive tract.
A helpful tool assembled by Northeastern University researchers is an online database called TrueFood (currently still a prototype) that lets you browse for common food items and brands to see how processed they are. Foods are scored on a scale from 0 to 100 for comparison purposes.
The last few years have been anxiety-producing for many people, and the inflation of food prices has only added to the burden. I hope these tips help you realize there are successful practices for eating a healthy diet without blowing your budget.
To learn more about how you can benefit from the First Mile Care Diabetes Prevention Program, take the prediabetes risk test and get started today!
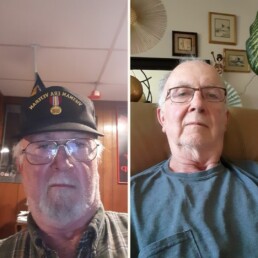
Q&A With DPP Participant: Group Support Helped Me Lose Over 50 Pounds
By Juliana Ronn, First Mile Care Director of Operations
Rickey Breeding is a 69-year-old auto mechanic and U.S. navy veteran. He is now retired from Ford Motor Company and lives in Redford Township, a suburb of Detroit. He joined the year-long First Mile Care Diabetes Prevention Program (DPP) in August 2022.

Rickey, you’re nearly finished with the First Mile Care DPP. What results have you seen so far?
- I’ve lost more than 50 pounds — specifically 55! In the past, I weighed as much as 265. My goal when joining the First Mile Care program was to get under 200 pounds and stay there. I’ve accomplished that.
- My A1C is now solidly in the normal range according to my doctor, at 5.4. Before starting the DPP, I was at 5.7, which is borderline prediabetes.
- My clothes didn’t fit when I started the program, and they still don’t fit – but now they’re baggy, which is a lot better than being too tight!
2. What made you join the First Mile Care Diabetes Prevention Program? Did you have a diagnosis of prediabetes?
My doctor with Henry Ford Health System, who is now retired, used to tell me regularly that I needed to lose weight. My A1C nudged into the range for prediabetes last year, and I knew I had to do something to become healthier. I was tired of being overweight, having tight clothes, and just not feeling well. I recognized that I was at risk for developing diabetes and I’ve seen what that does to a person. My girlfriend took medication for diabetes, which ran in her family, and experienced other chronic health conditions aggravated by her diabetes. I saw the ordeal she went through and decided it was time to get serious about lifestyle change so that I don’t put my eventual caretakers through a similar experience. I wanted to reverse my prediabetes before it turned into full type 2. So when I got an email from First Mile Care inviting me into the DPP, I was already in the mindset that I needed to take action. I checked with my current physician, Dr. Lubna Manzoor, and enrolled in the program.
3. What type of weight loss or lifestyle change programs have you tried in the past?
When my girlfriend developed cancer, I quit drinking soda and lost about 20 pounds. Unfortunately, that change didn’t last and I gained the weight back. I realize now that my issue is that I just ate too much and too many calories, all the time. I always cleaned my plate, no matter how big it was, especially when I dined out.
4. Why do you think the First Mile Care program is working for you when others haven’t?
First Mile Care provides you with the tools, knowledge, and guidance to lose weight and get control of your A1C. What I like is that it puts the responsibility into your hands. You decide how to apply the tools and knowledge to your own personal situation. You set your own goals.
The in-person aspect of the First Mile Care group meetings is really, really important to me. It’s not a burden to attend the meetings, as they’re held only 10 to 15 minutes from my home. I like seeing the other group members and sharing information. I want to be able to show success at each meeting. I don’t want to be the only person who gained weight instead of losing, or who isn’t meeting my goals. It’s an incentive to keep pushing ahead.
5. What are some changes you have made as a result of what you’ve learned in your DPP classes?
- I walk over five miles a day (10,000 steps) with my dog and sometimes as much as ten miles. I’m retired, so I have the time. I use a wrist device that tracks steps and distance.
- I dine out now a lot less than I used to. I’ve learned to eat more slowly and mindfully, and to stop eating when I feel full. It used to be that I never left food on my plate but ate every last bite. Now I leave the food or ask for a takeaway bag.
- I still eat pizza, but only once in a while instead of a couple of times a month, and I get thin crust so I’m eating less bread.
- I have always liked vegetables, but I eat a lot more salad than I used to, and I often buy pre-mixed salads at the grocery store.
- I’ve quit buying potato chips and instead eat baby carrots as a crunchy snack.
- I’ve cut way back on sugar. I’m more careful of the sugar in fruit, and I’ve given up drinking sugary soda. I mix up sugar-free drinks or teas instead.
6. What do you enjoy most about the First Mile Care program?
The group dynamic. The camaraderie. Being in the same boat. Having an all-for-one attitude. Maybe it stems from my military background that I like working within a team towards a common goal — to get healthy. While each person is held accountable for their own success, we also want the group to succeed. I want to see each person meet their goals and I personally don’t want to let the group down. I’m going to miss the meetings when I finish the program. When the time comes for the class to end, I hope we’ll exchange contact information and stay in touch.
7. How is the DPP group dynamic?
My group has only a half-dozen people, both men and women. We have a good time, kid around, are supportive, share stories, and encourage each other. We get along really well, despite being from different backgrounds. For example, I’m white, while the others in my group are not. However, most of us work or used to work for Ford Motor Company, so we have that in common. We all live in the same general area, so have the same frame of reference and share information on local places to shop and eat. We spend a lot of time talking about what to eat, how to fix it, and where to get the ingredients.
When the program started, I was the only person who was considerably overweight. The other folks have had less weight to lose, under 20 pounds, but are still at risk for diabetes due to family history. So it’s been interesting to be in the class. In some ways, I’ve had it easier. I’ve been focused on losing pounds and seeing the numbers on my scale change. I get quick positive reinforcement from that, and “attaboys” from the others in the meeting when I report my weight loss. The others have had to work harder to see change since they had less weight to lose. They’ve had to establish other rewards and success measurements than just weight loss.
We encourage each other. I’m motivated by hearing other people’s success stories, and I know that my own story, and that of my girlfriend, has encouraged other folks who were struggling to continue in the program.
8. What role has your coach played in your success?
Coach Kara Torres is always giving encouragement. The program and the handouts let us know that it’s OK if you slip up and that everyone needs a little encouragement at times. She pays attention to what we say we’ve eaten and offers advice. For example, I had no idea how much sugar is in a banana! I also used to drink a glass of orange juice every day at breakfast, thinking it was good for me. Coach Kara made me aware that a single glass could have the juice — and sugar — of as many as five oranges in it! I wouldn’t dream of eating five oranges in one sitting. So, instead of drinking a glass of juice every day, now I eat an orange instead. It’s been an easy way to reduce my sugar intake while still getting my vitamin C and enjoying the taste of the fruit itself.
9. Do you expect to maintain the progress you have made in changing your lifestyle?
Yes, it’s not hard with the food app and the activity tracker that Coach Kara taught us to use. I find it helpful and easy, so I’ve continued with tracking even though we’re not required to do so. I feel so much better now that I can’t imagine letting myself backslide.
- I use the Nutritionix app (www.nutritionix.com/app) to log my food intake. It automatically estimates calories. I try to stay under 2,000 calories a day and the app alerts me if I’m close or go over. I also eat salad now a couple of times a day, and can estimate pretty well in my head how many calories even if I don’t log it into the app.
- I also have an activity watch that keeps track of how many steps I take daily, and how many calories I burn. My dog pesters me for long walks so it’s not hard for me to meet my activity goals.
- I try to stick to my healthy eating during the week, but will allow myself a little treat on the weekend as an incentive. My group talks a lot about ice cream and how a little is OK. It’s all about moderation.
10. What advice do you give to people asking you about joining a lifestyle intervention program like First Mile Care?
I tell people my personal story, of how my girlfriend struggled with her diabetes and how her experience inspired me to take control of my health. It’s not easy to change your habits, but if the alternative is developing type 2, you can find the motivation. For example, one of the people in my First Mile Care group didn’t think he could stick with the program, but he reconsidered after hearing my story. If you have prediabetes, you should do everything possible to reverse it while you still can.
To learn more about how you can benefit from the First Mile Care Diabetes Prevention Program, take the prediabetes risk test and get started today!
Healthy Meal Prep in the Age of Inflation, Part 1
By Jenny Fowler, First Mile Care DPP Coach
Food prices have shot higher in the last year than most of us have ever experienced. The USDA Consumer Price Index for grocery store food purchases was 8.4% higher in March 2023 than one year earlier. The cost of food has increased for multiple reasons, including overall inflation, labor shortages, avian influenza, the Russia-Ukraine War, residual pandemic-related supply chain issues, and weather-related emergencies such as droughts, flooding, and wildfires.
The decisions you make when food shopping can be tough these days. Do you buy the item that’s best for your budget, for animals, for the planet, for farmers, for local markets? What wins out when you are forced to choose between your values, your taste buds, and your pocketbook? The First Mile Care Diabetes Protection Program (DPP) recognizes there’s no one-size-fits-all approach to healthy eating. Our coaches counsel DPP participants to find a balanced diet made up of nourishing, whole foods, heavy on vegetables and fruits, that works for their particular palate and lifestyle.
The good news is that with some smart shopping practices and a few substitutions, you can eat healthy, appetizing food and stay within your budget. In this two-part article, I’ll provide some tips that can help with your meal ingredient purchasing decisions, as well as how to make meal prep at home faster and thereby more practical for our busy lives.
Efficient prep practices
Restaurant spending is up around 40% from four years ago, according to U.S. Census Bureau data. Despite higher prices, Americans are continuing to dine out, with 61% in a recent survey saying it’s for convenience and 28% saying they don’t have enough time. Herein lies the conundrum, as my top tip for eating healthy, budget-friendly meals is to prepare meals at home as much as possible.
Home cooking has gotten a bad rap, as many people think cooking is too difficult, time consuming, and expensive. The COVID crisis gave many folks the gift of time to rediscover the rewards of preparing home-cooked meals. Getting the whole family in the kitchen cooking together helped fill the void from the loss of our usual face-to-face connections and community activities.
It’s a reality of life that you’re less likely to cook a meal spontaneously after a long, busy day. In an ideal world, I’d get all my meal prep done during the weekend for the coming week — chopping vegetables, dicing fruit, mixing salad dressings, roasting nuts and meats, etc. That makes it much faster to fix a healthy meal during the week, rather than starting from scratch each day and prepping as you go. However, the reality is that Sunday meal prep is not always practical for everyone. Weekends are often full of activities or just a time for relaxation and rest. Downtime is an important part of a healthy lifestyle, too!
Here are a few tips to make prepping healthy meals easier throughout the week.
- Choose an easy recipe like overnight oats or chia seed pudding that you literally just mix the ingredients together and put in the fridge. It’s very quick prep time and it lasts for days in the fridge.
- Plan at least two meals from the same ingredients so you save on shopping time and don’t waste your food budget. For example, roast a sheet pan of chicken and vegetables for dinner one night, then add leftover chicken and roasted veggies to salad greens or already cooked quinoa for the next day’s lunch.
- Meal prep doesn’t have to follow a recipe! Keep canned goods on hand like beans, salmon, or tuna, and fun salad toppings like artichoke hearts. You can throw these together and add fresh salad greens or leftover vegetables to complete the meal. Changing the herbs or spices you add to the same basic ingredients can also keep things from getting boring.
- Open an extra can and double your recipes so you won’t have to cook as often. However, have a plan for your leftovers so they don’t sit in the fridge too long and then end up as wasted money in the trash.
Healthy eating does not have to break the bank, and is often easier on your wallet than a traditional burger. Planning your meals to fix at home not only makes it less likely that you’ll be tempted by the drive-through window, but may also help to cut down on food waste. Even if you’re a cook-to-survive person rather than a foodie, there’s a wealth of resources on the internet to help you develop a go-to archive of easy-to-make, nutritious, tasty recipes on a budget.
In Part 2, I’ll look at some smart strategies for food shopping.
To learn more about how you can benefit from the First Mile Care Diabetes Prevention Program, take the prediabetes risk test and get started today!
First Mile Care Earns CDC “Full Plus” Recognition for DPP
By Karl Ronn, First Mile Care CEO and Founder
We’re honored to share that First Mile Care has been awarded “Full Plus Recognition” from the Centers for Disease Control (CDC) for our National Diabetes Prevention Program (DPP) lifestyle change program. This designation is reserved for programs that meet CDC standards for delivering a quality, evidence-based program that achieves retention thresholds.
As a critical member of the national effort to prevent diabetes, First Mile Care already achieved “Full Recognition” status in 2021. The new “Full Plus” status means that the sustained success of our lifestyle change program has earned us five years of CDC recognition moving forward.
“It is programs like First Mile Care that are turning the tide in the fight against the epidemic of type 2 diabetes,” wrote Miriam T. Bell, team lead of the National Diabetes Prevention Recognition Program at the CDC, in a letter announcing the designation. “It is immensely gratifying to see the science of diabetes prevention being implemented to improve the public’s health. Thank you for your commitment to reducing the preventable burden of diabetes in the U.S.”
An important benefit of Full Recognition status is eligibility for enrollment in Medicare as a Medicare Diabetes Prevention Program (MDPP) supplier. As a CDC-recognized in-person organization that has already achieved Full Recognition status, First Mile Care is able to bill Medicare for in-person DPP services provided to eligible beneficiaries.
To achieve this CDC distinction, the First Mile Care team had to meet stringent requirements in a number of categories:
- Lifestyle curriculum content
- Staffing and training
- Intervention duration and intensity (frequency of sessions over one year)
- Minimum percentages for session attendance over the year
- Documentation of body weight
- Documentation of physical activity minutes
- Average weight loss of a minimum of 5% of starting body weight across all participants in the year-long cohort
First Mile Care already teams with health care providers in the greater metropolitan areas of Houston, Detroit, Ann Arbor, Syracuse, and San Francisco. We’re also expanding into Chicago and Central California. More than 600 people enrolled in the First Mile Care DPP in 2022, and our goal for 2023 is at least 1,000 participants. (See testimonials on our website from a few of our successful graduates.)
Health systems and community-based physician practices interested in offering First Mile Care DPP to their patients should contact us for more information.
To learn more about how you can benefit from the First Mile Care Diabetes Prevention Program, take the prediabetes risk test and get started today!
3 Deep Breathing Techniques for Managing Stress
By Gray Jessiman, First Mile Care DPP Coach
Breathwork or active breathing has become a popular component of wellness programs in the last few years because of its many health benefits. Like meditation, active breathing can reduce stress and anxiety, promote better sleep, and improve symptoms of depression. Breathwork can be a useful technique for people with prediabetes who are trying to lose weight to address their glucose (blood sugar) levels.
In the First Mile Care Diabetes Prevention Program (DPP), our coaches counsel participants on stress management as a component of a healthy lifestyle. Stress increases inflammation, the foundation for almost all chronic diseases. The relationship between stress and weight loss is important to understand. When the body is experiencing stress or anxiety, the stress releases hormones that cause the body to elevate blood sugar, store fat, and have a more difficult time burning fuel for energy.
When you are in a stress-producing situation, the sympathetic mode of your nervous system takes over, releasing adrenaline and causing your heart rate to race and your blood pressure to rise. As you experience this acute “fight or flight” mode, your appetite may be temporarily suppressed. But if the stress becomes chronic, it causes a release of cortisol which may affect your appetite and could create food cravings.
Moreover, just the mere fact that you are stressed will elevate your blood sugar. Therefore, the more time you spend being stressed, the more time your glucose level remains high, which becomes a health issue over time. Learning coping mechanisms, identifying the connection between your moods and your snack cravings and adopting good sleep hygiene to bring down your stress level, are all key to maintaining normal blood sugar. You may not be able to change the stress-provoking situation, but you can change the way you react to it.
One mechanism for better managing your emotional state is controlled breathing. Many types of breathing involve long exhales, which slow the heart rate and help to relax a person. This kind of breathing affects the parasympathetic mode of your nervous system, also known as the “rest and digest” mode. During this time, blood pressure goes down, heart rate slows, and stress hormones decrease.
“Breathe, breathe in the air …”
Specific breathing exercises are used for therapeutic purposes including relaxation and improving well-being. Exercises may include changing the breathing depth, such as deep or shallow breathing. It can include changing breathing rate, i.e., how quickly or how long it is done. Additional breathing exercises include changing the way air is inhaled, either through the mouth or the nostrils, and other components of breathing that control different body parts, such as relaxing or contracting the stomach.
Andrew Huberman of the Huberman Lab has shown the science behind various types of breathing. Box breathing, cyclic sighing, and cyclic hyperventilation are three types of breathing that can help you to reduce stress and feel more balanced and grounded in your everyday life. The first two are easy to do and do not require supervision.
- Box breathing is a simple inhale, a pause, and an exhale. You inhale for three to four breaths, pause for three to four breaths, and exhale for three to four breaths. As the name implies, it is a simple method and can be easily implemented.
- Cyclic sighing works very quickly in real time. Cyclic Sighing is one big long inhale through the nose, followed by a short, sharp inhale, and then a slow exhale through the mouth. This type of breathing balances the carbon dioxide in the body and has been shown to be the most effective in reducing stress.
- Cyclic hyperventilation has a similar effect to cyclic sighing, but the initial breathing is a very active breathing that increases adrenaline and epinephrine and activates the autonomic arousal state of the nervous system. When you do this, you have more carbon dioxide in your blood and are in a slightly hyperventilated state. You may experience a tingly sensation and feel a little agitated, but the end result after this type of breathwork is a feeling of calm.
However, it’s important to be aware that this type of breathing exercise is best done under the supervision of an experienced facilitator, as you could experience dream-like images. Some people have even reported that this type of intensive circular breathing helps them explore their unconscious mind and heal from trauma.
If you’re participating in the First Mile Care Diabetes Prevention Program and are interested in using breathwork to help improve your emotional balance and well-being, try exploring these breathing techniques. Experiment with box breathing first, and then move to cyclic sighing, and track how they help you to relax and reduce your stress levels. “Take a deep breath” is a simple but effective piece of advice that is easily practiced at any stage of life.
To learn more about how you can benefit from the First Mile Care Diabetes Prevention Program, take the prediabetes risk test and get started today!
Developing Healthy Snacking Habits
By Barbara Martinez-Benavides, First Mile Care DPP Coach
America is a nation of snackers. According to Statista research published in January 2023, around half of the U.S. population says snacking serves as a meal replacement both at home and at work. Our long periods at home during the COVID-19 pandemic led to explosive growth in the sales of processed snacks like cookies, chips, popcorn, and pretzels. Luckily, as the pandemic has waned, consumers are now showing a growing interest in healthier types of snacks.
There isn’t a hard-and-fast rule about snacking that applies to everyone. How much you snack depends on your individual biology and lifestyle. One thing that is important across people, though, is to stay curious on why you feel you need to snack throughout the day. In the First Mile Care Diabetes Prevention Program (DPP), our coaches ask: What’s triggering your snack cravings?
Ask yourself these questions:
- Could I feel hungry because I’m not getting enough quality sleep?
- Did I recently change my diet? Am I eating mindfully?
- Do my meals include all the macronutrients my body needs? Am I getting the right amount of filling foods such as fiber and whole grains?
- Am I drinking enough water, especially if I’ve been exercising?
- Do I have really long days that are making me tired?
- What’s my mood? Am I feeling stressed, bored, lonely, or sad?
“If I’m preparing for an important work-related call, I notice that I want to reach for a snack,” said Jeff Millhouse, who completed the First Mile Care program in Texas. “I ask myself: ‘Am I truly hungry, or anxious, or perhaps not hydrated enough?’ Sometimes just having a glass of water will suffice. I realize I associate food with relieving boredom or providing a sense of comfort.”
Mike Kowis is also a successful graduate of the First Mile Care DPP. “When I sit down in the evenings to watch TV, I used to have a snack like popcorn or ice cream. After our discussion of triggers and habits in a First Mile Care session with Coach Sandra Huskey, I realized that I eat at night because it’s just what I do as a routine, triggered by turning on my favorite talk show. So I have learned to stop myself from opening the refrigerator or cupboard and instead ask myself, am I really hungry?”
Heck, you might even think you’re hungry because you were subconsciously influenced by a TV commercial!
Food, glorious food!
If true hunger really is the reason you’re craving a snack, go for something nutritious, like vegetables, fruits, nuts, or seeds, rather than bombarding your body with a large meal or, heaven forbid, heavily processed chips and cookies with empty calories.
When you’re deciding on a snack, bio-individuality plays a huge role here again. What have you been eating throughout the day? What are you doing the rest of the day — jogging or binging TV?
Here are some low-calorie yet filling foods that work well as healthy snacks: carrots, celery with salsa, cottage cheese, cucumbers, dill pickles, a hard-boiled egg, Greek yogurt, or roasted vegetables (e.g., broccoli and cauliflower cooked with olive oil spray).
I recommend including at least two food groups as part of your snack, for a more satisfying experience and to help you feel full for longer. For example, plain yogurt with berries, apple with almond butter, carrots or celery with hummus, a rice cake with guacamole, or a square of dark chocolate with an apple, are quick snack options.
“I’m a night owl and sometimes snack late at night, but now I eat carrots and celery at Coach Taylor Winkel’s suggestion,” said Olidia Thomas, who participated in the First Mile Care DPP in Michigan.
If you want to get more creative with your snacks, check out these linked recipes: blueberry bites, chia pudding, fruit ice cream, crispy chickpeas, kale chips, and veggie trio salad.
Mike Kowis added, “If I want something salty and crunchy, I might substitute a raw carrot stick and sprinkle on a tiny amount of salt. I’m still getting that salty taste that I crave, but am also eating a healthy snack with vitamins instead of the empty calories in popcorn. It might sound weird to substitute carrots for popcorn, but it works for me!”
Now for the bad news …
If you’re trying to lose weight or just get healthy even when weight isn’t an issue, there are several common snacks that aren’t as healthy as you might think, and could even stall your progress towards weight loss (if that’s your goal).
Nuts. The high protein and fiber content of nuts make them a satisfying snack, but quantity and quality really matter. Nuts are already high in fats and calories, and then oftentimes have added flavors, oils, and salts which pack on more calories. If you nibble on the right portion, nuts make a great snack option, but it’s easy to over-indulge.
Smoothies. The healthiness of a smoothie depends on the ingredients you put in it. Some people add up to five different fruits, plus honey, plus toppings. If you make the smoothie yourself and keep it simple — one fruit, some greens, water, etc.) — it can be a healthy and filling snack option. Beware, though, that if you buy a smoothie, it could have even more calories than a milkshake. Check out First Mile Care Coach Sandra Huskey’s article on hydration with tips for creating healthier, satisfying smoothies.
Veggie chips. Just because the name is “veggie” doesn’t make them healthy. They don’t have fiber, so they won’t keep you full for long periods of time. They usually contain similar ingredients to regular potato chips — oil, sodium, preservatives, and other additives — so they are still high in calories.
As a general rule of thumb when it comes to snacks, be wary of misleading labeling. Some snacks labeled as “healthy,” “keto,” and “low carb” may indeed be good options, but many processed foods are disguised as healthy by buzzy marketing terms like “gluten free,” “low fat,” or — in the case of chips — “baked.”
Closing advice
I recommend keeping at least two healthy snack options available and ready at home, work, and in the car. If snack meal prep at home is an option for you, that is a great way to set up yourself for success. When you do your food shopping, make sure you have at least one healthy snack on your grocery list, and ideally, in an individual or “personal” size so you’re not tempted to overeat when you open the packaging. It’s even possible nowadays to find healthy snacks like fruit, nuts, and salads in gas station markets — but always read nutrition labels carefully to avoid high calorie snacks. (You’ll find advice on interpreting nutrition labels in this article.)
First Mile Care DPP participant Al Cisneros offers this insight. “I’ve become attuned to where empty calories are placed on shelves. If I go into a convenience store, there are doughnuts nearby, or candy by the cash register. Instead of giving into sugar cravings, I walk a couple of aisles back and find a healthier snack like unsalted nuts or celery sticks.”
My final takeaway when it comes to snacking is an easy one, and usually costs nothing — always, always drink water before snacking. Not only will you know if it is indeed true hunger that you’re experiencing and not thirst, but the water will help fill you up so you may eat less of the snack.
To learn more about how you can benefit from the First Mile Care Diabetes Prevention Program, take the prediabetes risk test and get started today!
Q&A With DPP Participant: Healthy Eating Habits for Disease Prevention
By Juliana Ronn, First Mile Care Director of Operations
Deborah Wilson joined the year-long First Mile Care Diabetes Prevention Program in April 2022. She agreed to talk about why she joined, the results she has seen, and her tips for leading a healthier lifestyle. Deborah is a retired 58-year-old living in Detroit, Michigan who spent her career working with special needs children.

1) What was your biggest health-related problem before joining the First Mile Care Diabetes Prevention Program?
My weight had been fluctuating up and down for about a year and a half. Since I’m vegetarian, I found it difficult to figure out how to eat. I confided in my doctor, Dr. Sarala Vunnam at Henry Ford Health Systems, and told her I needed to see a nutritionist. That’s when she told me about First Mile Care. I didn’t want my health to go from bad to worse and I didn’t want to go on a “diet.” I wanted professional help with lifestyle change to figure out what was right for me.
2) Now that you’re finishing the program, how do you feel about your eating habits?
Along with being vegetarian, one of my biggest challenges was a lack of appetite. I would go all day not eating because I didn’t have a big appetite. Coach Gray Jessiman encouraged me to take pictures of when I was able to eat a balanced meal so that it would motivate me to eat. For meals, I make my plate bright with pretty colors and that motivated me the most. I make sure vegetables take up half the plate to make the times I do eat big meals really count, to provide the energy I need. When I don’t feel like eating, I make a smoothie because I know that will satisfy me. It was all about finding ways to eat that worked for me.
I love to snack on nuts but can unknowingly eat a whole bag in one sitting. Becoming aware of correct portion sizes by preparing snacks in containers was a really helpful tip from Coach Gray. I even use a smaller plate when I’m fixing meals to avoid overeating, so I’m much more conscious about how I prepare my plate overall.
3) Did you know what prediabetes was before First Mile Care?
Yes, I had first-hand experience with type 2 diabetes as my father went into a diabetic coma and never came out. So I was quite aware of what diabetes was all about and that has made me very adamant about monitoring my own health. While I don’t exactly know if I had a prediabetes diagnosis before joining the program, I knew I was at risk for diabetes due to my family history, so I needed to learn how to maintain a healthy weight and avoid developing bad habits. It wasn’t that I was overweight, I just wasn’t at a weight that was comfortable for me and I knew what I wanted for myself because I’d seen my father pass away.
4) What measurable changes have you seen since completing the program?
I joined the program at 159 lbs. My tests showed that everything was fine but my whole life I had been 20 lbs lighter and I had noticed post-menopausal weight gain. With my familial experience with type 2 diabetes, I didn’t feel comfortable at that weight and knew I needed a change.
Now that I’m finishing the program, I’m between 147 and 150 lbs which I am very happy with. I’m still working on getting to 139 lbs, but when I went to check-in with Dr. Vunnam this year, all of my tests came back great! So, yes, through changing my diet and reducing my weight, I feel successful in preventing diabetes.
5) What did you most enjoy about the First Mile Care program?
I liked working with Coach Gray because she understood me and she was great at personalizing the program for me. It was helpful to have one-to-one support to get her input on food labels and she provided recommendations if I should buy a product or not. If I needed extra help, she had lots of ideas and recipes to try but I never felt any pressure. She let me make my own choices. It all boiled down to figuring out a way for me to eat food that would align with my goals and she helped me figure it out.
6) What role did your coach play in your success?
Coach Gray really customized the program for me, my goals, and my health situation. In 2009, I received a diagnosis for a rare muscle disease that kept me in a wheelchair for several years. It’s a disease only 1% of the population has so, in terms of a solution, the doctors don’t know how to treat me. Through determination and the support of my family, I’ve been able to move without a cane or a walker for a few years now. My muscle disease aside, I also experience hip pain at times.
Being able to understand my triggers is what has kept me out of the wheelchair. Now that I’ve mastered my eating, including movement in my lifestyle is key. If I go on a walk, I make sure to listen to my body and take short breaks. Before the pandemic, I was going to the gym once or twice a week and my goal was to try to walk 10,000 steps daily. Now, I spend hours gardening and I’m getting 7,000 or 8,000 steps every day just through growing tomatoes (I have 15 different types!), green beans, strawberries, peas, watermelon, cantaloupe, squash, cucumbers, bell peppers, and lemon peppers.
Coach Gray knows my challenges and was the one who told me that, with my disease, I should be careful about eating too many tomatoes or bell peppers. That was something I didn’t know but I’m a tomato lover! I am so determined this won’t just be a year-long program but a full, permanent lifestyle change for me. It was just those little personal things that my coach recommended that have made all the difference for me in being able to sustain my new habits.
7) Was it helpful to have people in the same geographic area as you embarking on lifestyle change?
Yes! The majority of my group was based around the east side of Detroit, and in our weekly discussions it was helpful to chat about which local stores people could find different ingredients, like monk fruit, and being able to strategize with your group about where to find specific ingredients or produce. It helped us to relate to each other by providing another level of support.
8) Did you find a food journal or another type of tool to be helpful?
I kept a food journal in the beginning and then stopped once I had developed the eating habits that worked for me. Right now, I’m on a salmon kick where I’ll eat salmon, corn, and broccoli for about a month straight, and journaling helped to build that habit. We also built action plans about eating and exercising that I try to follow when I can. However, because of my physical challenges, sometimes I’m in too much pain to walk so I just have to listen to my body and do what feels right.
9) Did you learn something that was surprising from the program?
I learned that walking 10 minutes after you eat is a good way to burn more sugar. Coach Gray also recommended eating my food, waiting, and then drinking water after eating, to avoid slowing my digestive system. Lastly, I’m very good at reading food labels now and learning that if you can’t pronounce it, don’t eat it!
10) Do you think you’ll be able to maintain these habits after the program?
Absolutely. The only challenge has been learning how to eat out at restaurants. I know what to order but sometimes the meals will come with sides where I don’t know the ingredients or the calorie count. I learned that my solution is to just eat around it.
Everything I learned from First Mile Care I live by and I tell people about it. Sure, sometimes I’ll have my cheat days but I’m much more aware of a lot of my habits. I do tell a lot of people about what I’ve learned because when I teach other people, it sticks with me. I’m very adamant about keeping my weight down and now it’s a lifestyle, so it will be very natural to maintain these habits.
To learn more about how you can benefit from the First Mile Care Diabetes Prevention Program, take the prediabetes risk test and get started today!
Get on Your Feet! 8 Tips for Breaking the Deadly Link Between Sitting and Prediabetes
By Sandra Huskey, First Mile Care DPP Coach
There is mounting research connecting sedentary lifestyles to an increased risk of diabetes, dementia, and heart disease as people age. Some experts have even referred to sitting as the new smoking — it has the potential to be that deadly!
According to the Centers for Disease Control and Prevention (CDC), more than one out of every three adults in the U.S. has prediabetes, and nearly half of adults have high blood pressure — conditions aggravated by long hours of physical inactivity. Luckily, simple movement and exercise can help mitigate the negative health effects associated with extended durations of sitting.
In the First Mile Care Diabetes Prevention Program (DPP), coaches advise participants to get at least 150 minutes of moderate-intensity physical activity each week. Coaches recommend you keep track of how much time you spend sitting still each day, for a few days, to have a baseline number for comparison. You will probably be surprised to find that even when you get 150 minutes of activity a week, you spend an awful lot of time sitting still — especially if you have a desk job.
Check out these tips if you’re trying to build habits to incorporate movement breaks.
1. Find a fitness activity you like. Try going for a walk outside, 5-minute yoga, or even a dance break (like this BeeGees one or this Elvis one). Be honest with yourself about your enjoyment level of the activity. You’ll find an excuse to stay sitting down if you’re trying to avoid the movement you have planned!
2. Break it up. Sometimes it’s easier to find small chunks of time throughout the day than one giant period of time. The DPP recommends two minutes of movement for every 30 minutes. Researchers at Columbia University Medical Center recently published a study in the journal Medicine & Science in Sports & Exercise that showed even a five-minute walk every half-hour can help control blood sugar and undo a lot of the risks incurred by sitting for long periods.
3. Create times to move. Taking a movement break might not come naturally in your busy life. You may need to set a timer to remind yourself to stand up and walk around every half-hour until it becomes a habit.
4. Invest in a treadmill or standing desk. On the days that inclement weather doesn’t allow an outside walk or life becomes too busy to disconnect, a treadmill can help maintain your habits. Some people have set up their desks around a treadmill to encourage walking while working and taking meetings. In that way, you don’t have to choose between productivity and your health. There are even space-saving under-desk treadmills and walking pads, too. If you must remain seated at a desk, try sitting on an exercise ball which allows some bouncing movement.
5. Take a stretching break. If the cold, heat, or humidity isn’t in your favor or you’re not feeling up to your usual movement, try taking a stretch break. Stretch breaks will help reduce muscle tension and increase blood circulation. Static muscles will fatigue easily and stretching will help you become comfortable (and make tasks less difficult)!
6. Multi-task. Too many items to cross off your to-do list? See if you can combine your errands with movement. For example, if you live within walking distance, step out on foot to the grocery store or post office. Hold standing or walking conference calls with co-workers, or make a rule that you’ll only allow yourself to phone a family member while you’re on your feet. Create a new habit of always walking in place during the opening credits of your favorite TV show, or during a comedian’s opening monologue. If you use public transportation, stand instead of grabbing a seat, at least for a few stops.
7. Make it engaging. Turn up the music or your favorite podcast during activities. You’re more likely to build and maintain a new habit if it’s coupled with something that you already look forward to doing, and listening to energizing music can help you move faster without realizing it. If you’re into video gaming, a virtual reality (VR) headset may get you on your feet and moving around as your mind is tricked into entering immersive simulated environments.
8. Build in a healthy reward. There’s no better way to encourage a habit than positive reinforcement when you achieve a goal. Maybe there’s a movie or TV show you’ve been wanting to watch or a special purchase you’ve put off. After incorporating movement breaks in your day, a reward is definitely earned!
Take the advice of Gloria Estefan — get on your feet! Get up, stand up, and take some action to promote healthy aging.
To learn more about how you can benefit from the First Mile Care Diabetes Prevention Program, take the prediabetes risk test and get started today!
What’s the Best Trendy Diet Program? (Hint: It’s the One That Works for You)
By Taylor Winkel, First Mile Care DPP Coach and Registered Dietitian
Did you know that the word “diet” comes from the Greek word “diaita,” which means “way of life”? Diet can mean both habitual nourishment, what you normally eat and drink, as well as an eating regimen specifically designed to promote weight loss.
In the First Mile Care Diabetes Prevention Program (DPP), our coaches emphasize eating for healthy aging. We teach that diet, weight loss, and healthy eating are connected, but not interchangeable. Weight loss is a natural side effect to ongoing lifestyle change that involves healthy eating and exercise, but it takes time to achieve.
It’s very common that our DPP participants ask coaches: What’s the best diet? Do you recommend the [Atkins, DASH, IMF, Keto, Nordic, Paleo, Pritikin, Whole30, Zone, etc.] diet? Which one do you think will work for me?
What I tell my group participants is, diets are not one-size-fits-all and there is no magic formula to weight loss. What works successfully for one person may be challenging for someone else. Some popular diets may help you to drop weight in the short term, but aren’t healthy overall and are so restrictive that they become impossible to maintain. The best diet, therefore, is the one that works for you in the long term and promotes sustainable healthy habits.
Fads versus facts
U.S. News & World Report recently announced its annual ratings of popular diets. An expert panel analyzed and ranked 24 diets across several categories. The list examines diets that have some basis in science and avoids some of the more wacky diets and TikTok trends. For the sixth year in a row, the Mediterranean diet came out on top.
The Mediterranean diet is really a style of eating rather than a restrictive diet, focused on simple, plant-based cooking — good quality fruits and vegetables, whole grains, beans and seeds, a few nuts, and olive oil as the preferred fat over butter. Fish is emphasized rather than red meat, while eggs, dairy, poultry, sugar, and refined foods are eaten less than in the traditional Western diet. An important lifestyle part of the diet is eating mindfully and socializing with friends and family over meals.
Denial is a commonality among many of the diets in the U.S. News rankings. That can be their downfall as restriction generally does not work over time. The more complicated and restrictive a diet, the harder it becomes to keep to it. Who wants to live a life in perpetual denial? When you’re fixated on weight loss, you’re more likely to develop an unhealthy relationship with food. Instead, focus on adding only quality calories and ingredients to promote wellness.
Here are a few key points that First Mile Care coaches recommend:
- Eat well-balanced meals of unprocessed whole foods. Non-starchy vegetables should account for about 50% of your plate, lean protein foods for about 25%, and the remaining 25% of carb foods like starchy vegetables or whole grains or fruit.
- When possible, cook at home so you can control ingredients, calorie quality, and portions.
- Read nutrition labels so you know what you’re eating and serving sizes.
- Keep hydrated with water and not sugary drinks.
In addition, a healthy lifestyle includes exercising daily (at least 150 minutes of moderate activity per week), getting adequate, high quality sleep, and managing stress.
Check out the U.S. News & World Report rankings to see their expert evaluations of popular diets, including meal plans, food lists, and tips.
You may also want to watch the webinar about “Deconstructing Popular Diets” on our blog.
To learn more about how you can benefit from the First Mile Care Diabetes Prevention Program, take the prediabetes risk test and get started today!
Q&A With DPP Participant: Becoming Accountable for Lifestyle Change
By Juliana Ronn, First Mile Care Director of Operations
Patricia “Pat” Bagozzi joined the year-long First Mile Care Diabetes Prevention Program (DPP) in May 2022. Pat is a retired 70-year-old widowed grandmother of four living in Westland, Michigan, a suburb of Detroit. She spent 35 years as a claims representative with the AAA Auto Club of Michigan, so knows something about the importance of listening carefully to other people’s problems.
Pat, you’re now about three-quarters of the way through the First Mile Care DPP. What results have you seen so far?
- Normal A1C. My blood sugar is in the normal range again! When my doctor tested my A1C level four months into the program, it was in the normal range at 5.7. One year earlier, it was at 6.0 so indicated prediabetes.
- Healthy weight. I’ve lost 46 pounds and feel fantastic! I’m pretty much at my goal weight now and am feeling good about myself. And it’s not been hard. I put on three pounds over the holidays yet was able to lose it fairly quickly in the new year.
- Healthy girth. I have dropped two clothing sizes. I always used to buy loose flowing tops to cover my upper body. Now I can wear skinny jeans and fitted sweaters and pants with zippers instead of elastic waists! I am so confident about keeping the weight off that I’ve given away my old clothes or had the more expensive items tailored.

What made you join the First Mile Care Diabetes Prevention Program? Did you have a diagnosis of prediabetes?
I didn’t know specifically that I had “prediabetes” although my doctors at Henry Ford Health Systems warned me about losing the extra weight around my midriff and lowering my cholesterol and A1C. My previous doctor told me I had certain markers I needed to get under control, although she also knew my family situation with my husband’s illness, and told me not to try to take on too many changes at once. While a member of my family has gestational diabetes, I was never really too concerned about developing type 2, but as a former smoker, I knew I was at risk for heart disease.
After my husband passed away, I knew it was time for a big lifestyle change. I spent years putting other people first. I was always busy but I wasn’t really focused on myself. I took care of my husband, my work, my kids, and my grandkids. So when that phone call came from a First Mile Care representative, asking to send me information on the Diabetes Prevention Program, I knew it was time to take care of me and put my needs first — for the first time in decades.
I had already quit smoking and drinking, but I was sitting a lot and doing a lot of mindless eating, so I kept putting on weight, ballooning to as much as 200 at one point. After I had knee replacement surgery in the fall of 2020, I could start walking more, which really has helped in losing weight.
What type of weight loss or lifestyle change programs have you tried in the past?
I tried Weight Watchers but I found their points system confusing. It also costs a bit, and people seem to have to go to it for years. I don’t want to deny myself anything. I want to be able to eat what I want when I go out with friends, and not be one of those people who brings my own dish or asks other people to adjust what they’re serving to accommodate me.
Why do you think the First Mile Care program is working for you when others haven’t?
What the First Mile Care program does is make ME accountable for what I put in my mouth and for the healthy food that I eat and for the type of exercise I get. But nothing is off limits and nothing is mandated – apart from getting 150 minutes of exercise a week. Coach Taylor Winkel told me to pick something to do in terms of activity, my choice as to what, just as long as I got the minimum time in. The program has also given me the incentive to read nutrition labels and make sure that everything that goes in my mouth has a purpose. I allow myself to eat what I want, but pay attention to quantity and nutrition, so I’m more satisfied at the end of the day.
What are some changes you have made as a result of what you’ve learned in your DPP classes?
I faithfully read food labels and note the calories, servings sizes, and portions to prepare healthy meals. What’s the amount of added sugar, does it have whole wheat, is it processed? Honestly, I couldn’t believe the amount of food that I was eating before I started the DPP! I used to love eating potatoes and starches that turn into sugar. I’m surprised that I didn’t weigh more than I did, because it was nothing to me to eat a whole big bag of chips in one sitting. While I may eat some chips now, it’s a small package, not a whole bag.
I continue food journaling to track what I eat and drink. I use a watch with a health tracker to record my activity and remind me to move occasionally. I also use the MyFitnessPal app on my phone for gauging and tracking calories. I monitor my water intake, as that’s super-important. I always look at menus online now before I eat in a restaurant with friends, so I can make a conscious decision about what I eat and how much. I’ll only eat half of what I order, have a few chips, have a glass of water, and take the rest home.
What do you enjoy most about the First Mile Care program?
There are a couple of things — education and camaraderie. This program offers one-on-one individual advice. You make the decisions. You set your goals and action plans. You figure out with the coach, through education and trial and error, what works for you as an individual, which may be different from what works for other people. I also enjoy the program for the sense of camaraderie I’ve built with the other people in my group. That’s what I’ll really miss once I’ve finished the program — and hope I can stay in touch with some of the folks. We really do talk about our issues. We give suggestions to one another to work around our challenges.
How is the DPP group dynamic?
There are a couple of things — education and camaraderie. This program offers one-on-one individual advice. You make the decisions. You set your goals and action plans. You figure out with the coach, through education and trial and error, what works for you as an individual, which may be different from what works for other people. I also enjoy the program for the sense of camaraderie I’ve built with the other people in my group. That’s what I’ll really miss once I’ve finished the program — and hope I can stay in touch with some of the folks. We really do talk about our issues. We give suggestions to one another to work around our challenges.
What role has your coach played in your success?
First Mile Care has given me the tools and information to understand healthy options, and to help guide me to make the right choices for me and develop behaviors that promote wellness. Each person is different, so it’s all about finding the right balance of what works for the individual. It’s really helpful that Coach Taylor is a foodie and a registered dietician (RD). She really knows her stuff and has educated us on getting healthy amounts of fruits and vegetables in our diets, and explained what different nutrients do in your body. She turned me onto eating Greek yogurt and helped me adjust my bread consumption. She has helped me to understand that if I’m not hitting the goal I’m striving for, I need to adjust the type and amount of food I’m eating, and to vary the kind of exercise.
Do you expect to maintain the progress you have made in changing your lifestyle?
Absolutely! I’ll never go back to the way I was, mindlessly eating and never getting any exercise. I’m positive about that. I’m a determined person. That’s my personality. Monitoring what I eat, eating healthily, and exercising has become a habit, just like putting on a safety belt when I get in a car.
My main exercise is walking and using exercise bands. I started using them to strengthen my knee after surgery, but now also use them for stretching and arm curls. They’re easy to take with me if I’m away from home. My walking routine lapsed recently when my dog had surgery and it was really rainy outside. Even one week of not walking makes a difference. Now I’m trying to work more weights into my daily routine, and I might sign up with a gym to be able to do water aerobics and other classes in the future.
What advice do you give to people asking you about joining a lifestyle intervention program like First Mile Care?
This program is a whole change of mindset and something that becomes your habit. You have to have the “will to wanna” make a change. But once you see results, you can’t get enough of it. It has really been a metamorphosis for me — I’m like a butterfly! At 70, I can’t wait for my grandkids to come over to the house and I can go-go-go with them. I’m thankful for it every day and speak about it everywhere I go. It’s a beautiful thing.
To learn more about how you can benefit from the First Mile Care Diabetes Prevention Program, take the prediabetes risk test and get started today!






















